Stay safe post-flood! Visit here to learn more about how to stay safe.
TRAFFIC ADVISORY: NVHD IS OPEN DURING CONSTRUCTION ON RT. 67.Traffic may temporarily be re-routed to enter the parking lot from Martha St. during construction.
Stay safe post-flood! Visit here to learn more about how to stay safe.
TRAFFIC ADVISORY: NVHD IS OPEN DURING CONSTRUCTION ON RT. 67.Traffic may temporarily be re-routed to enter the parking lot from Martha St. during construction.
MERS represents a very low risk to the general public in the United States. Only two patients in the U.S. have ever tested positive for MERS-CoV infection—both in May 2014—while more than 1,300 have tested negative.
Middle East Respiratory Syndrome (MERS) is an illness caused by a coronavirus called Middle East Respiratory Sydrome Coronavirus (MERS-CoV). Most MERS patients developed severe respiratory illness with symptoms of fever, cough and shortness of breath. About 3 or 4 out of every 10 patients reported with MERS have died.
The disease was first reported in Saudi Arabia in September 2012. According to the CDC, so far, all cases of MERS have been linked through travel to, or residence in, countries in and near the Arabian Peninsula. The largest known outbreak of MERS outside the Arabian Peninsula occurred in the Republic of Korea in 2015 however, the outbreak was associated with a traveler returning from the Arabian Peninsula.
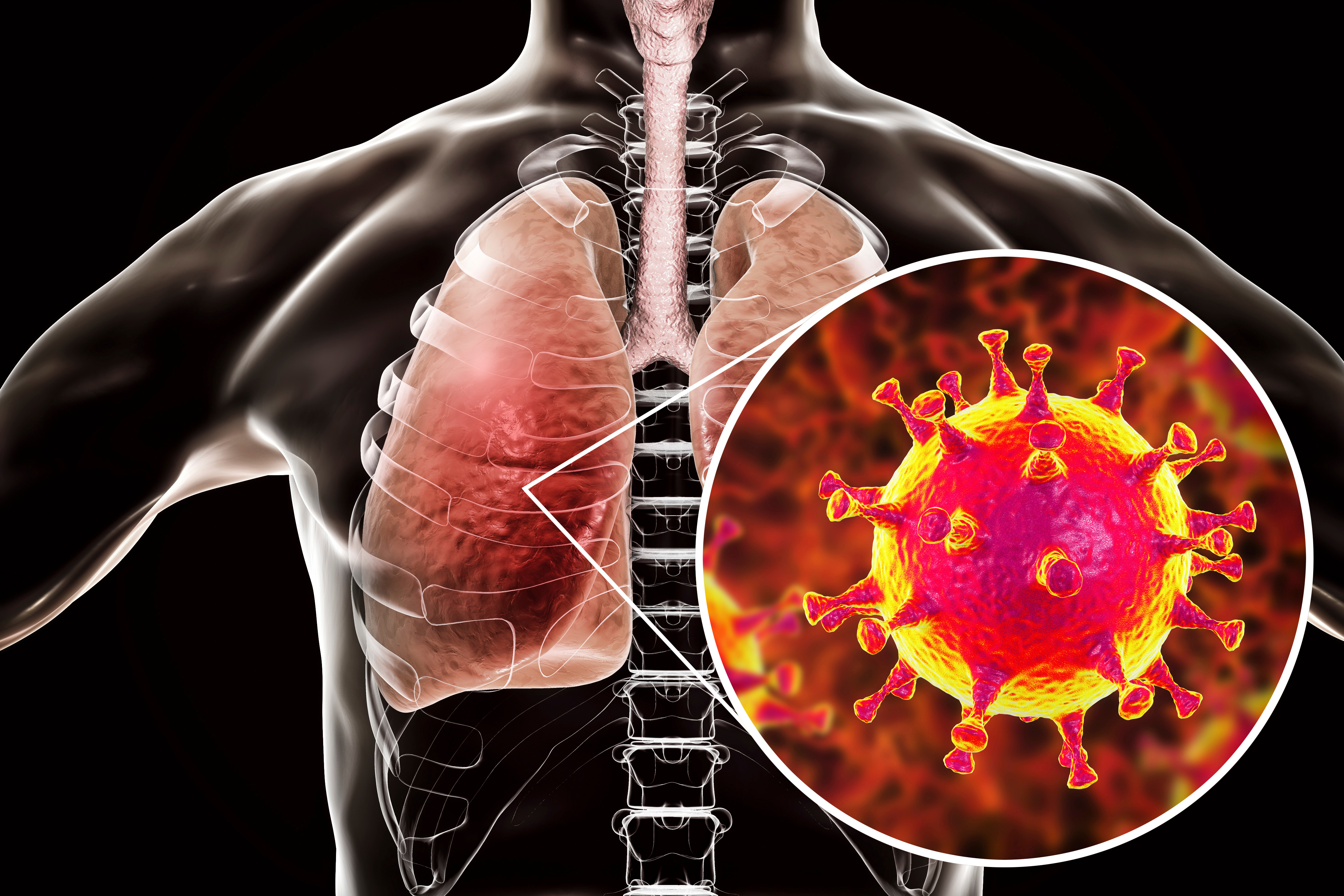
Most people confirmed to have MERS-CoV infection have had severe respiratory illness with symptoms of:
Some people also had diarrhea and nausea/vomiting. For many people with MERS, more severe complications followed, such as pneumonia and kidney failure.
About 3 or 4 out of every 10 people reported with MERS have died. Most of the people who died had a pre-existing medical condition that weakened their immune system, or an underlying medical condition that hadn’t yet been discovered.
Pre-existing conditions among people who got MERS have included
Some infected people had mild symptoms (such as cold-like symptoms) or no symptoms at all.
The symptoms of MERS start to appear about 5 or 6 days after a person is exposed, but can range from 2 to 14 days.
MERS-CoV, like other coronaviruses, likely spreads from an infected person’s respiratory secretions, such as through coughing. However, the precise ways that it spreads is not yet fully understood.
There is currently no vaccine to protect people against MERS. There is also no specific antiviral treatment recommended for MERS-CoV infection.
You can help reduce your risk of getting respiratory illnesses:
If you are caring for or living with a person confirmed to have, or being evaluated for, MERS-CoV infection, see Interim Guidance for Preventing MERS-CoV from Spreading in Homes and Communities.
Individuals with MERS often receive medical care to help relieve symptoms. For severe cases, current treatment includes care to support vital organ functions.
If you think you may have been exposed MERS-CoV, see People at Increased Risk for MERS.